Event Description
Oregon State Public Health Laboratory Shares Lessons Learned from Its Newborn Screening Program
Description:
The history of newborn screening (NBS) demonstrates the strength and integrity of its mission: to identify children with congenital conditions who need treatment to prevent adverse outcomes. NBS started in just a few states screening for a single disorder – phenylketonuria - and has grown to a core panel of 37 conditions. It is anticipated that the panel will continue to evolve as the knowledge of genetic conditions expands, detection technologies advance, and new treatments emerge. Join this OneLab Network event to learn more about the newborn screening system and how the state of Oregon has advanced its NBS work to improve health outcomes in babies across the state.
Objectives:
After completing this training, participants will be able to:
- Identify educational and other resources available through the OneLab Network
- Summarize the history of newborn screening as well as the current newborn screening system
- Describe new developments in newborn screening
Attendees may be eligible to receive 1.0 contact hours of P.A.C.E.® credit.
Event Speakers
Keynote Speakers

Dr. Patrice K. Held, Ph.D
Manager of Oregon Newborn Screening Program
Oregon State Public Health Laboratory
Co-Director of the Biochemical Genetics Laboratory
Oregon Health & Sciences University
Event Media
Event Media
Audio Transcript
07.25.23_OneLabNetworkEvent_Recording
CHELSEA PARSONS: Hi, everyone. Thank you so much for joining us for this OneLab Network event. We're going to give it one more minute for attendees to join, and then we'll go ahead and get started.
All right, let's get started everybody. My name is Chelsea Parsons. And I'm a consultant with Guidehouse, supporting CDC's OneLab Initiative.
I just have a couple of notes to run through before we begin the webinar. If you're having any technical issues throughout the session at all, you can feel free to email our OneLab inbox. It's onelab@cdc.gov. That's onelab@cdc.gov. You'll see that email address just posted in the chat.
If you have any questions throughout the session regarding the session materials, you can place those in the Q&A function. You'll see that in your bottom ribbon of your Zoom box right now. There's a Q&A function. Please submit questions in there throughout the entirety of the session.
We will take 10-ish minutes at the close of the session to go through our Q&A. We'll do our best to get to all the questions. But if you don't get your question in today or you'd like to reach out with additional questions following the session, you're more than welcome to also email us at onelab@cdc.gov.
Note that you'll see a link to live captions in the chat right now. That is available for anyone to use if you need it throughout the session. But we do ask that you keep this Zoom window open and the live captions window open in order to use it.
All right, so let's get into our agenda for today. We're just going to go through a few relevant resources that we have offered on OneLab. And then we'll introduce you to today's presenter. We'll have our main presentation. And then like I mentioned, we'll go into that short Q&A session at the end. And then our OneLab host, Alicia will give you an update on some of our upcoming events.
So with that, I will turn it over to our OneLab Network lead, Alicia Branch. And she will begin to share some of our new and relevant resources. Alicia?
ALICIA BRANCH: Thank you, Chelsea. As Chelsea stated, I will share some free helpful OneLab resources related to today's topic and state two disclaimers, followed by the introduction of today's presenter. DLS offers, again, free-- three free-- e-learning courses related to genetic testing, good laboratory practices for molecular genetic testing, good laboratory practice recommendations for biochemical, genetic testing, pre-analytic phase, and establishment and validation of new tests using liquid chromatography, and biochemical genetic laboratories. Next slide.
In addition, to the free e-learning courses, we also offer free job aids available in PDF and Word format, such as "Genetic Testing, What You Need to Know, Health Professionals," and "Genetic Testing, What You Need to Know," and the top 10 recommendations for laboratories performing molecular genetic testing. Next slide, please.
The slide decks may contain presentation material from panelists who are not affiliated with CDC. Presentation content from external panelists may not necessarily reflect CDC's official position on topics covered. Next slide, please.
CDC, our planners and our presenters wish to disclose that we have no financial interest or other relationships with the manufacturers of commercial products, suppliers of commercial services, or commercial supporters. Next slide.
And now, I'm excited to introduce Dr. Patrice Held, our presenter for today. Dr. Held manages the Oregon Newborn Screening Program-- excuse me-- overseeing the testing and followup units. Additionally, she co-directs the biochemical genetics laboratory at Oregon Health and Science University. Dr. Held has been rooted within the newborn screening public health system for over 12 years and is currently chairing the Association of Public Health Laboratories Quality Assurance, Quality Control subcommittee. Our speaker for today is Dr. Patrice Held.
PATRICE HELD: Hello, everyone. I'm hoping that you can see my slide deck. And first, I want to thank you for--
ALICIA BRANCH: You can't see it yet.
PATRICE HELD: Oh. Check. Great. I want to thank you for the warm welcome. As was mentioned, I serve as the Newborn Screening Program manager in the state of Oregon.
I'm really excited to talk with you today because newborn screening is celebrating 60 years. The program first began in 1963. And here we are in 2023.
So I'm hoping that my presentation will cover a bit about the history of newborn screening, the operational activities of our current newborn screening programs, as well as the future direction of newborn screening. And over the course of my presentation, I'm hoping to highlight previous successes, current challenges, and lessons learned.
CHELSEA PARSONS: Hey, Patrice, we do not see your slides right now.
ALICIA BRANCH: We can't see your screen, your slides.
PATRICE HELD: You do not. OK. Can you see-- OK, I'm sorry.
ALICIA BRANCH: No, you're fine.
PATRICE HELD: Now do you see them?
ALICIA BRANCH: We do.
PATRICE HELD: OK. And you see the side that says, What Is Newborn Screening?
ALICIA BRANCH: Yes.
PATRICE HELD: OK. All right. So what is newborn screening? Newborn screening is a state public health program. All states have a newborn screening program. And many countries also have a newborn screening program.
And the goal of the newborn screening program is to identify infants with treatable conditions that may otherwise go unrecognized. So all of the conditions on our newborn screening panel has specific treatments. And all of them require a laboratory test or an intervention in order to identify the children with the conditions. And of course, the ultimate goal is to be able to provide treatment before the onset of symptoms in order to prevent adverse outcomes. And just after-- the CDC selected 10 public health achievements in the 20th century. And newborn screening was named one of those achievements within the category of healthier moms and babies.
So what are our newborn screening statistics? There are nearly 4 million babies born in the United States each year. And 97% of them are screened through a newborn screening program. And we know that this has led to over 12,000 babies each year whose lives have been saved or improved because of this screening. In Oregon, we have approximately 40,000 births each year. And over 100 babies are diagnosed with one of the conditions on our newborn screening panel.
So a little bit about the history of newborn screening, and really you have to go all the way back to the early 1900s. So in 1908, Sir Archibald Garrod, an English physician really pioneered the field of inborn errors of metabolism. He understood that diseases were oftentimes the result of missing or false steps in the body's biochemical pathways.
He specifically studied alkaptonuria and cystinuria. And later, a lot of his findings were published in the first version of the book, Inborn Errors of Metabolism. And really, he laid the groundwork for the idea of the molecular basis of disease.
It wasn't until 1934 that Dr. Folling described phenylketonuria. So Dr. Folling recognized that a set of symptoms that included intellectual impairment, motor problems, and skin abnormalities were also associated with an abnormal amount of phenol pyruvic acid that was being excreted in the urine. And so he described phenylketonuria.
And then in 1951, Horst Bickel discovers the treatment for phenylketonuria. That in a diet that is devoid or depleted of phenylalanine, that children with PKU would not present the phenotype. That the intellectual impairment would be improved, as well as the motor and skin abnormalities.
So together these three men laid the foundation for Dr. Robert Guthrie to come in. And Dr. Guthrie developed the bacterial inhibition assay in order to measure phenylalanine levels in dried blood spots. And you can see here on the figure on the right is in agar gel. And each one of these red circles is a dried blood spot from a different baby. And his assay was designed such that the bacterial growth would be exponential if there was an excess of phenylalanine. So here, this one sample has x excess phenylalanine that led to the growth of the bacteria.
And so using this technology, he was able to screen many babies all at once. And so he basically took his assay on the road and went state by state, convincing states that it was less expensive to screen every baby, identify those with PKU, and treat them than it was for the state to care for a child with PKU who was untreated. And it worked.
In 1963, five states, including Oregon, passed laws that required universal screening for PKU. And I highlight Massachusetts here because not only did Massachusetts pass the law, but they also initiated screening for all babies. It wasn't until 1965 that Oregon was able to achieve screening for all babies born in the state.
And this middle field here is an old filter paper card blood spot that was collected in 1972. That was used for PKU screening within the Oregon newborn screening program.
So I put in this slide here to, again, pay tribute to Dr. Guthrie. This is a blog that his daughter put together for him and his work. And he is known for saying that no child should die or suffer disabilities if a simple blood spot test could prevent it. And one of his colleagues designed this cute little image that his work was one small step for a man, but one giant leap for mankind.
So again, in the 1960s is when newborn screening began. And most states began to screen for only PKU. It wasn't until the 1970s that states started to add on additional tests, additional diseases. Sickle cell disease was added, along with congenital hypothyroidism. And then in the '80s, an additional set of diseases were added, galactosemia, maple syrup urine disease, congenital adrenal hyperplasia, and biotinidase deficiency.
And really these seven disorders maintained newborn screening programs for a long time until the early 2000s. And what happened in the early 2000s was the introduction of tandem mass spectrometry to the newborn screening programs. And tandem mass spectrometry really revolutionized the way that we do newborn screening because from that simple blood spot punch, we would be able to screen for many conditions all at once. And so many more inborn errors of metabolism were added-- amino acid disorders, organic acidemias, and fatty acid oxidation defects. There was an explosion of conditions.
Also in the 2000s was the addition of our first molecular test, severe combined immunodeficiency, and also our first point of care test for hearing loss. In the 2010s, states brought on screening for spinal muscular atrophy through another molecular-based assay, as well as screening for lysosomal storage disorders and one peroxisomal storage disorder, and also added on yet another point of care test for critical congenital heart disease. Since then in 2022, states have added on screening for mucopolysaccharidosis type 2 and in 2023 screening for GAMT deficiency.
In May of 2010, so going back a little ways, there was the creation of the national Recommended Uniform Screening Panel. And the RUSP is a list of conditions that are ready for screening. And it can serve as a guide for newborn screening laboratories. The Recommended Uniform Screening Panel is supported by the HRSA Advisory Committee on Heritable Disorders in Newborns and Children. And all of the conditions have been recommended by the Secretary of Health and Human Services.
So at present there are 37 core conditions on the RUSP. And it is recommended that all states screen for these conditions. In later slides, I will describe the review process for how conditions are added to the RUSP.
I think one of my most valuable lessons that I learned about newborn screening very early on was that newborn screening isn't just the laboratory test. It isn't just that bacterial inhibition assay that Dr. Guthrie designed years ago. But really newborn screening is an entire system and that each step within the system is critical and necessary in order to achieve a successful public health program.
We must have prenatal education to inform parents and providers about newborn screening. And I highlight the website Baby's First Test here because that's an excellent resource for expecting and new moms about newborn screening.
We need to have adequate and timely specimen collection. Typically, the specimen collection is performed by hospitals, nurses or phlebotomists, or performed by midwives who are delivering out of hospital births.
We need to have timely transport of the specimen from the point of collection to the laboratory, the public health laboratory. And of course, we need to do our testing well and report the results in a timely manner.
On the flip side of testing is really the post-analytical pieces of the program. That encompass both short-term followup and long-term follow up. So as you know, this is a screening test. So any screening result that the laboratory generates needs to have confirmatory testing performed to confirm the presence of the disease. And short-term followup ensures that every screen positive result has a definitive diagnosis.
And then the long-term followup is really the care that is given to the child that is identified with the condition over time so that we can ensure that those children are meeting the appropriate milestones and are never lost to followup. In Oregon, that portion of the program, the long-term followup, is done by our medical center in the state, Oregon Health Sciences University.
This is what our newborn screening card looks like in the state of Oregon. And the newborn screening card is, again, filled out by nurses and phlebotomists or midwives. Every field is important and necessary in order to perform our testing well.
And on the right-hand side, you see what the blood spots would look like on the filter paper. And this is an image of what we would say a high quality or good quality blood collection. Some of the images in the lower portion of this slide represent blood spots with incomplete saturation. So the circle is not completely filled, or images of a specimen with blood clots on it. So it is optimal to have a good quality specimen in order to have a good quality result. And we spend a lot of time working with submitters on how to collect the specimen appropriately.
We also work a lot with our submitters on how to fill out the card. Key information, like birth date and time, collection date and time, or babies birth weight, as well as the formula or the food source that the baby is receiving, if the baby is in the NICU, has the baby been transfused, all of this information is necessary for us to appropriately interpret our laboratory results.
And then the last field that's important on the card is this lower one, which is asking the hospital or the midwife to identify, who is the PCP? Who is going to be the baby's pediatrician? And who should our results be communicated to?
Once that specimen card is completed and the blood is being collected, then it needs to be transported to the laboratory in a timely manner. And back in the late 2013, there was a new series of news stories that came out about newborn screening, in which it was titled, "Deadly Delays." And what it was focused on was the idea that hospitals were collecting the samples in a timely manner, but they weren't making them to the laboratory in a timely manner. And so this delay in transport led to an inability to report results in a timely manner and an impact to children who had the disease.
And so, again, this added to the concept that newborn screening is an entire system. And something like specimen transport, which may not necessarily seem significant, was truly impactful to our mission. And it's something that the public health program needed to be aware of and to monitor.
At the same time, HRSA got involved with their advisory committee and put together recommendations for the timeliness of newborn screening. It is recommended that the blood spot be collected within 48 hours after birth of the baby. That specimen should be received at the laboratory within 24 hours of collection. And that all results should be reported within seven days of that baby's life.
We know that results for time critical conditions-- so these are the most severe conditions on our panel-- actually need to be reported within five days of life in order to have optimal outcomes. Versus the time sensitive conditions, those that are less severe, can be reported within seven days of life.
And so using these recommendations, we now have a really condensed timeline where birth of the baby is happening on day 0. Specimens need to be collected between day 1 and day 2. Transport to the laboratory within a single day, ideally laboratory testing done on day 4, with results reported by day 5.
So what type of technology is used within the newborn screening laboratories? So I mentioned that we screen for hemoglobinopathies. And I think this is probably one of the lab staff's favorite tests to perform. It's an isoelectric focusing gel that allows for the identification of hemoglobinopathies by the separation of the variant forms of hemoglobin.
So we know that in a newborn baby they should have both fetal hemoglobin and adult hemoglobin. A baby with sickle cell disease will have only fetal hemoglobin and sickle hemoglobin. And those with sickle cell trait will have both fetal, adult, and sickle. Or those with C trait will have fetal, adult, and C.
So again, this is a very visual test that we perform in the laboratory. It's very hands on. But you also get to see a nice picture of your results.
Another type of technology that we use in the laboratory is an immunoassay. And we use an immunoassay to screen for hypothyroidism, congenital adrenal hyperplasia, and cystic fibrosis. And the way that this testing system works is that we're able to identify and quantitate the analyte of interest by binding it to an antibody that has a fluorescent tag that allows for detection. So in the case of hypothyroidism, we are looking at the levels of thyroid stimulating hormone through this immunoassay setup.
As I mentioned earlier, we screened for many of our inborn errors of metabolism through the use of tandem mass spectrometry. So this is an image of a mass spectrometer. And again, we are able to use the mass spectrometer to look for multiple different analytes all at once in a single dried blood spot.
And then over the years, we've incorporated more and more molecular techniques. So I mentioned quantitative PCR is used for severe combined immune deficiency, as well as for spinal muscular atrophy. And I suspect in future years the incorporation of more and more techniques to the newborn screening laboratory.
So I wanted to insert this slide again to reiterate the screening platforms that we use. So when we are screening for phenylketonuria, we are measuring phenylalanine or tyrosine. So we are measuring the metabolites. We are not looking at the actual enzyme activity, which we know to be deficient in people with PKU, nor are we looking at the gene sequence for this enzyme and detecting variants we are again measuring the metabolites so we're measuring a biochemical phenotype.
Now, not all of our assays, but a majority of them, look at this biochemical phenotype. A few of our assays do actually measure the enzyme activity for other diseases. And again, we have a couple of molecular assays that look at that gene sequence.
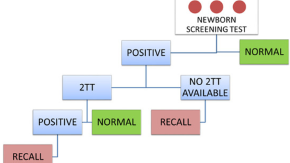
So when we think about reporting our newborn screening results, we like to think about it in the context of risk assessment. So we're measuring this analyte. And if that analyte of interest is elevated above or below a cutoff, we would say that the baby-- that the result-- that the baby screens positive for the disease and is at high risk for the disease. However, additional diagnostic testing is needed to confirm the presence or the absence of the disease. And when we have a screen positive result, we notify health care providers to take the next appropriate steps.
If the analyte that we measure is within the range that we determine is the range of the unaffected population, then we would say that the baby screams negative for the disease and they are at low or a negligible risk for the disease. It doesn't mean that they don't have the disease. It is still possible that they might have the disease, but the risk is very low and no additional action is needed at that time.
We occasionally have inconclusive results where we find ourselves being unable to reliably detect or measure the analytes of interest. And in those situations, we ask for a repeat screen.
So when we look at our screening test performance, we need to consider the range of analyte concentrations that we might obtain. So when you think about the normal population, the unaffected population, and the concentration of phenylalanine in those individuals, it's certainly a bell curve, where some will have low concentrations of phenylalanine and some will have higher concentrations of phenylalanine. Yet they will all be denoted as the normal population, the unaffected population.
And the same is true for the affected population. Those with the presence of the disease will have a range of concentrations. And I'd say in a perfect world, these two distributions would be completely separate. The normal population distribution would be separate from the affected population distribution.
However, that's pretty much never the case. So what we find ourselves is the two populations overlapping. And we need to set a cutoff, a value of the analyte or, in the example of phenylalanine, a threshold level where if you're above this level, then you screen positive. And if you're below the level, then you screen negative.
And so when we try to set those cutoffs, we know that we are at risk for false positives within the unaffected population. And we know we are at risk for false negatives, so missed cases within the affected population. So we struggle a lot with newborn screening laboratories to try to figure out where is the appropriate place to set that cutoff.
And one of the ways that we have helped improve our performance is through the use of multiple tiers of testing. So we might perform a first tier test to take the whole population and to narrow it down to identify those that are at risk and separate those that screen positive versus those that screen negative. And then within the screen positive population, we would perform a second tier test, or another test, to again whittle down that population into a smaller group of people that are, again, most likely to be at risk for the disease. And it's in that population that we would then refer to medical care.
And cystic fibrosis is a really great example of how newborn screening laboratories have used these multiple tiers of approaches. So I mentioned that when we screen for cystic fibrosis, we use an immunoassay. And we measure immunoreactive trypsinogen. And we know that it's not a great marker for the disease. Immunoreactive trypsinogen can be elevated not only in individuals with cystic fibrosis, but in other physiological conditions.
And so what newborn screening laboratories have done is that they've implemented a second tier test where they are either sequencing the CFTR gene, or they're looking at common variants within the gene that are known to be disease-causing, so performing that second layer of testing. And from there, we're able to really hone in the population that is likely to be affected with cystic fibrosis. And again, all of this layers of testing is aimed at improving our screening performance.
So once we report out that screen result, the next step is to perform short-term followup. And our short-term followup unit that is housed within our newborn screening program, they are responsible for ensuring that all newborns receive a valid screening test and those with screen positive results receive a definitive diagnosis, either confirmed disease or false positive, in the most expedited manner possible.
Once the child is confirmed to have the disease, they enter long-term followup. And long-term follow up comprises the chronic disease management and condition specific treatment, along with age-appropriate preventative care through the life span of the individual.
So moving on, I wanted to talk about the current goals of newborn screening programs. So some of the things that we are working towards currently is harmonization between newborn screening programs. So we know that not all newborn screening programs use the same language to describe their results. Sometimes labs are using the words normal or abnormal. Sometimes labs are using the words screen negative or screen positive.
We also don't name our conditions in the same way. Nor do we count our conditions in the same way. So there's a lot of work to be done around harmonization of language and also harmonization around the diseases that are screened. I think it is potentially-- no, I think it is optimal that states, as best as they can, move towards using the recommended screening panel as their guide so that no matter what state your baby is born in they are getting the same conditions.
Another piece in which we can achieve harmonization is assessing the effectiveness or the quality of our programs, so to basically ensure that every baby, no matter what state you're born in, receives the same quality testing. And we can look at quality indicators to assess that that is actually occurring.
Another area for improvement in newborn screening is in education and outreach. We know that we don't always have effective communication and education about newborn screening to parents. Oftentimes, moms do not even know that newborn screening is occurring.
We also know that we have a lot of work to do to provide education and outreach to providers, whether that is reminding providers about the timelines around newborn screening and optimal specimen collection, or reminding providers about what screening results mean and how they are different than a diagnostic test. So I think there's many different work groups that are aimed at improving education and outreach within newborn screening.
Another place that improvements are needed is in long-term followup. So over the years, we've added conditions to our newborn screening panels that sometimes don't always present within the newborn period, but actually present a little bit outside of that newborn screening period, like maybe within the first year or two of life.
And so not only do we need to confirm the presence of the disease, but we need to monitor these patients long term to understand when the disease symptoms arise, when optimal treatment should be provided in order to really understand whether or not we are positively impacting the baby's life and achieving quality outcomes. So essentially long-term followup is a critical component of newborn screening programs to really understand the effectiveness of our programs.
And then lastly, a fourth current goal of newborn screening programs is in addressing health equity. So I think we maybe innocently assume that because every baby is screened that we've achieved health equity. But what we are now realizing is that even though 97% of babies are screened, not all of them have the same outcomes. And largely that is due to health inequities in our system.
So are they actually achieving a diagnosis in the timely manner? Are babies equally able to access treatment and equally able to access the care that they need? So again, taking that much more broader approach to the newborn screening program and looking at health equity, not just at the point of screening, but within the larger context.
So what are some resources that we have to help newborn screening programs? So the CDC plays a pivotal role in quality assurance. The CDC has a newborn screening quality assurance program that helps to develop analytical methods to measure different analytes in the dried blood spots. And they share those methods with the state newborn screening laboratories.
They also produce quality control material and reference materials to maintain quality testing. The CDC has initiated programs to look at harmonization of data across different testing platforms and across different laboratories. And this harmonization of data can help laboratories in setting cutoffs for their tests and interpreting results.
And one of the things that I think is most exciting is that the newborns-- the CDC has entered into a pilot program, that's titled ED3N. And ED3N is Enhancing Data-driven Disease Detection in Newborns. And so the idea of this pilot program is to combine that biochemical phenotype that we're measuring, the biochemical analytes that we're measuring, that data with the molecular data, the actual genetic variants that are present in the gene, and combining the biochemical and molecular data with the clinical data, the severity of the patient presentation. And I can imagine how powerful those three pieces together would be to really understanding the disease that we're screening for and the severity and the need for treatments.
Another resource that we have that helps newborn screening programs is provided by the Association of Public Health Laboratories. In their resource, NewSTEPS. So NewSTEPS was created by APHL as a resource center. And it collects data from newborn screening programs about quality assurance metrics and indicators about disease detection.
And it summarizes it for newborn screening programs so that we can understand how our program matches up to other programs and where there are needs for improvement. The other thing that NewSTEPS provides newborn screening laboratories is with technical assistance and training in the forms of webinars and toolkits, particularly around bringing on new conditions and what is needed for that.
So where is newborn screening headed in the future? And I think one of the main things that we have been working towards over the years is the addition of new conditions. So we know that there is an expanding number of conditions for which the molecular basis is known. There is over 7,500 different conditions that are known and over 4,800 genes that have been described with mutations that cause disease.
So we can only imagine that over time there's going to be more and more conditions that are ready or the molecular basis is known so that it would be optimal for screening, potentially optimal for screening. That combined with the rapidly growing list of therapies that are entering into market, so now you have a treatment.
So we anticipate that there'll be an explosion of conditions that are ready for newborn screening. Some of the ones that are currently either being considered or are actually being screened for in certain states include descend muscular dystrophy, Krabbe disease, and congenital cytomegalovirus.
So how do we know what diseases are ready for screening? So back in 1968, Wilson and Younger put together principles and practices of screening for disease. And this is a list of items to be considered for screening.
So is there a laboratory test for the disease, for screening? How rapid and reliable is that laboratory test? What is the positive predictive value of that screening test? And then in addition to the screening test, is there a confirmatory test available to confirm the presence of disease?
We also want to know whether or not the public health system infrastructure can support screening for the disease. Is there treatment available? Is there clinical care available? And is there counseling available?
When we're looking at the disorder, we want to understand the prevalence of the disease, the natural history of the disease, whether or not there's significant morbidity and mortality associated with the disease. Is there effective treatment? And will the treatment change the outcome or prevent the illness? And then lastly, the cost effectiveness of screening.
So these were some of the founding principles for how we add conditions to the panel. And as I mentioned, the Recommended Uniform Screening Panel is an outgrowth of the Advisory Committee on Heritable Disorders in Children and Newborns. And the advisory committee, again, takes each condition and undergoes an evidence-based review and then goes about a voting process to recommend the condition to the panel.
And that voting process looks at whether or not there's a significant benefit to screening, whether or not states are ready to screen, and whether it's feasible to screen. And I put this website here if you'd like to know more information about the actual process for adding a condition to the RUSP.
And we know that over time, there'll be emerging criteria for conditions. In the future, we will be more and more focused on the whole system. And this article bullets different criteria that will likely to be considered. So we will want to know that we are responding to a recognized need. We will need to clearly define the objective of our screening programs.
We'll need to integrate education, testing, and clinical services when we're onboarding new conditions. We need to start to allow for some autonomy or respect for the individual. We need to address more and more issues of equity and access to screening. And again, we'll always be weighing the benefits of screening to the potential harms.
So where else is newborn screening going in the future? So certainly, there'll be an introduction of new technologies. The use of whole exome or whole genome sequencing is just starting to touch into newborn screening laboratories.
And there have certainly been several different papers published about the use of whole exome or whole genome sequencing-- so the use of whole exome sequencing to identify inborn errors of metabolism, or the use of whole genome sequencing to really describe the differences between healthy and sick newborns. In other countries, specifically in England, there are pilot projects that are actively looking at screening newborns and understanding the utility of whole exome and whole genome sequencing.
Another potential place for new technology is in the use of metabolomics and proteomics to identify diseases. There are certainly been several papers published on the use of metabolomics, not only to identify inborn errors of metabolism, but also the use of metabolomics to identify biomarkers of disease that can be used to predict clinical phenotypes. So even though we're not quite there yet with newborn screening programs to use metabolomics, it's likely to become a future direction.
So given the expansion of new diseases and new technologies, where should we be putting our efforts into planning for the future? So one of the things that we think about is this continual request to add new conditions. And I think one of the things that I worry about is whether or not our current program infrastructure is able to handle additional conditions. What does it look like? Do we have the resources necessary to keep up with the addition of new conditions?
Another thing that I worry about is the impact of molecular technologies. So when we introduce these technologies, we will likely be able to detect more and more carriers of disease, and whether or not we should be reporting out carrier status. Within molecular testing, we know that we will identify variants of unknown significance-- so mutations where we do not know the impact of. And what do we do with those results? And likely also, we will need to understand how and when to provide information to physicians and parents on these results.
One of the things that we have not touched on yet is the idea of consent for newborn screening. Right now, most programs operate in an opt-out manner. So basically, newborn screening will happen unless the parent actively chooses to opt out.
And I guess I'm wondering is if this form of consent is adequate if we're thinking about implementing molecular technologies or adding more and more conditions to the panel. Perhaps, we might need to transition from an opt-out approach to an opt-in approach. And so that's another consideration for the future.
And lastly, there's considerations around the storage and the use of the dried blood spot specimens for research. What should we be using the blood spots for and the data for? And what types of research is appropriate or not appropriate?
So in the last 60 years, or maybe in the last, say, 15 years of my experience with newborn screening, what are some of the lessons that I've learned? Certainly, newborn screening is risk assessment. We are not diagnosing disease. But we are rather identifying newborns that are at risk or at a significantly increased risk for the disease. So it's a screening program for assessing risk. Additional testing will always be needed to confirm the presence of the disease.
As I mentioned previously, newborn screening is a system. It's not just a laboratory test. Each step of the process is equally important and necessary for a public health program. Education, outreach, short-term followup, long-term followup, all of them are critically important.
Another lesson learned is that quality assurance is absolutely necessary. And continuous quality improvement will always be occurring. We are always looking for ways to improve our newborn screening program, whether that is through metrics that monitor each step of the process, or whether it's looking at different types of testing or different staged approach to testing in order to improve the test performance.
Again, newborn screening foundation was equity-focused, in that every baby is screened. But in the future, we need to really think about the whole program and whether or not equity is truly achieved.
And lastly, a lesson learned is that change is inevitable and that newborn screening programs need to have ability, agility, and flexibility to respond to changes over time. So thank you very much. And I'm happy to answer any questions that you might have.
ALICIA BRANCH: OK, we'll go ahead and take a few minutes to answer as many questions as possible. If we do not answer your question today, we'll do our best to respond via email. If you have any questions after today, please feel free to email OneLab inbox at onelab@cdc.gov.
OK, I'll start with the first question. And this one's probably-- you probably can just really state how newborn screening programs are funded because the participant wanted to know how many screenings should be conducted for newborn babies? And what is the highest priority? And then they want to know because not many countries have the budget for this program.
PATRICE HELD: Yeah, that's an excellent question. So in the United States, the way that newborn screening-- there's different approaches for funding the newborn screening program. How it occurs in Oregon is that for our panel of roughly 40 conditions, we charge $175. Hospitals purchase the newborn screening cards from us, again $175 per baby. And then they use that card to collect the samples and send them to the laboratory for testing. Hospitals would then go on to bill insurance or Medicaid to cover the cost.
In other states, newborn screening programs might be funded off of different grants, like maternal health grants. Or they might be funded through the general funds of the state. In answer to your question, so I do not necessarily know how newborn screening programs are funded in other countries.
Let's see, your question was about the different diseases. So certainly within the United States, we have probably the largest panel of conditions in comparison to other countries. And other countries have selected diseases by their own criteria. And certainly some countries might select a disease because it has a higher prevalence or because of the cost, and again targeting diseases that are more severe or more prevalent in their population.
Did I answer all those questions?
ALICIA BRANCH: Yeah, I think so. I think that's the best you could do. Two participants kind of had something similar. One is like what's the most appropriate system for screening newborns in remote areas? And then the other one is do you have any experience implementing this program in a remote area?
PATRICE HELD: Oh, that's a really good question. So my experience is really limited to, let's say, the remote areas of Oregon. Or my previous place was in Wisconsin. And so I'm not sure that that's really considered remote in comparison to other countries, let's say. So I'm not sure I can answer that question for what that looks like in terms of other countries.
ALICIA BRANCH: That's fine. We'll do one more. What might the screening test results-- why might the screening test results sometime be inconclusive?
PATRICE HELD: Yeah, that's a really great question. So in the course of my slides, I showed you an image of the blood spots that were not really acceptable or of good quality. Either the filter paper wasn't completely saturated, so if you were going to measure the analytes, they'd likely to be very low in concentration because there just wasn't enough blood on the sample card. Or perhaps there's too much blood and blood clots, and you might get an increase in the concentration. So both of those scenarios would likely lead to inconclusive results.
Another place where we get inconclusive results is if the baby has received a transfusion prior to the collection of the sample. Then we may not adequately be able to detect the hemoglobin empathies, for example. Or if the baby is receiving total parenteral nutrition, that's highly supplemented in amino acids, then we won't really be able to get a good look at what the actual amino acid concentrations are in the baby. They might look elevated just because of the dietary intake at that time. And so that would also be an example of an inconclusive result.
ALICIA BRANCH: OK. I think that'll be all the questions for today. Again, for those who have questions, and you put yours in the actual question Q&A box as anonymous, if you could email us at onelab@cdc.gov, and we'll try to answer your questions. Again, that email is at onelab@cdc.gov.
Again, thanks again, Patrice. We are offering one PACE credit for today's webinar. To receive PACE credit, visit the link and passcode posted in the chat and complete the evaluation within two weeks. You will receive an email containing these instructions just in case you missed the link and the passcode before the event ends. Next slide, please.
To download videos from previous events, go to OneLab Reach Events Media tab and scroll to find the event you want to view. Videos and audio from our April and May events are coming soon. A link has been provided in the chat. Next slide, please.
Speaking of upcoming events, we want to highlight two OneLab Network events occurring in September. We have the CMS proficiency testing final rule, CMS 3355-F on September the 7th at 12:00 PM Eastern Standard Time.
And on September the 26th at 12:00 PM Eastern Standard Time, we have "How Clinical and Public Health Laboratory Professionals Should Plan for Possible Burkholderia Pseudomallei Exposure and Cases." This presentation is from an Arizona case study published in the May 2023 edition of the Emerging Infectious Disease Journal.
In addition, we want to highlight our OneLab Summit 2023, a three-day virtual learning event, titled "Thrive, People, Planning, Preparedness." It will occur on October the 3rd through the 5th. And registration details for the upcoming events are coming soon.
Again, as a reminder, the slides and links will be posted to reach.cdc.gov/onelabnetwork within the next two weeks. And thank you for joining. And have a great rest of your day.